Breast reconstruction is a surgical procedure that restores shape to your breast after a mastectomy — surgery that removes your breast to treat or prevent breast cancer. Breast reconstruction with flap surgery involves taking a section of tissue from one area of your body and relocating it to create a new breast mound.
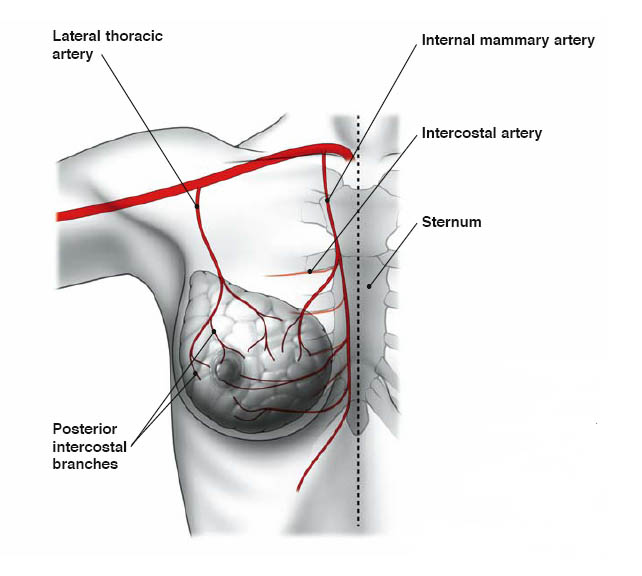
Reconstruction post mastectomy, can be achieved using one’s own tissue from another part of the body. This comes attached to its blood supple (pedicled flap), or the blood supply is reattached using microsurgical techniques (free flap). Autologous reconstruction uses tissue – skin, fat and sometimes muscle from another place on your body to form a breast shape. The tissue usually comes from the belly, the back, buttocks, pr inner thighs to create the reconstructed breast.
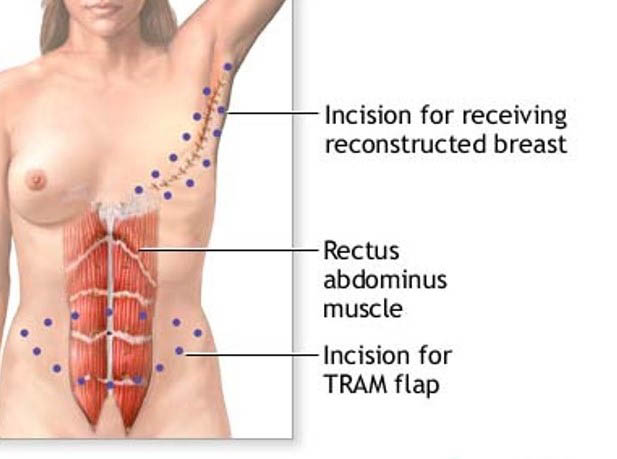
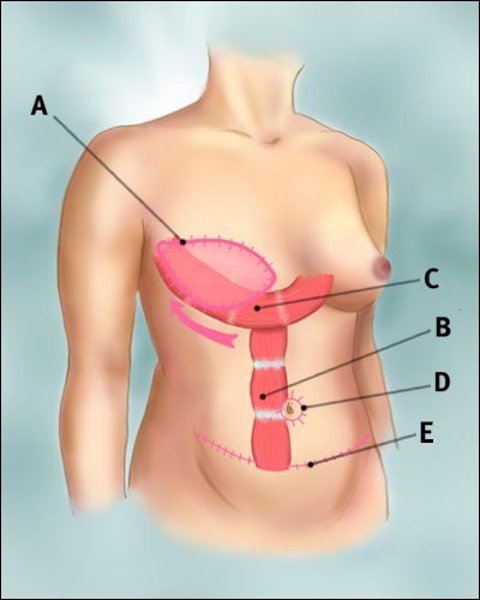
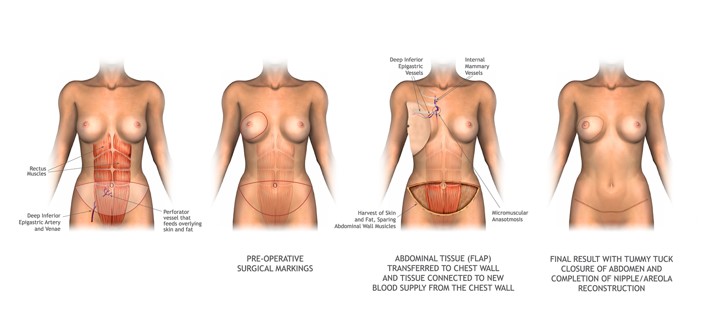
Many areas can supply tissue, depending on the volume required and if the blood vessel quality is adequate. Most commonly, tissue from the subcutaneous tissue of the lower abdomen is used. When it is attached to its blood supply it is referred by an acronym of the muscle used (TRAM – Trans Rectus Abdominal Muscular flap). When it is moved freely, it is referred to by the accompanying vessels (DIEP – Deep Inferior Epigastric Perforator Vessels Flap). Many women are please with using the belly tissue as it is like having a “tummy tuck” to rebuild a breast.
Surgical Methods
In summary Autologous tissue breast reconstruction uses one of two surgical methods:
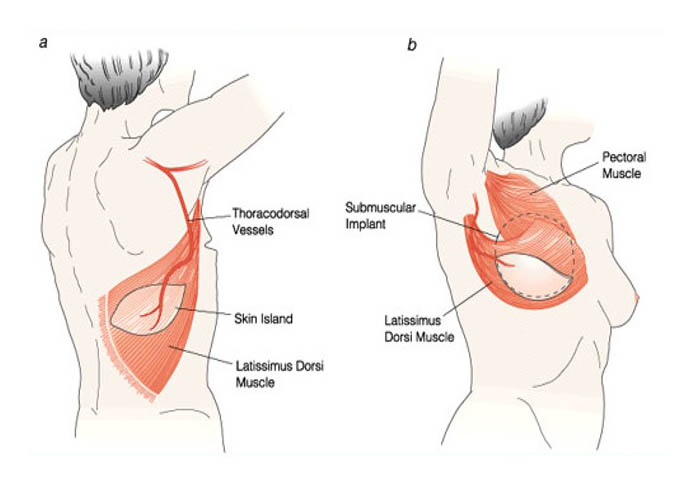
- Pedicled flap surgery – The surgeon cuts some of the blood vessels to the tissue to be transferred but keeps other blood vessels intact. Tunnelling the tissue beneath your skin to your chest area, the surgeon then creates the new breast mound or pocket for the implant. (see below images)
Details
Procedure:
- General Anaesthetic, ranges from 6-10hours.
- Generally, better to have two teams of surgeons to decrease the anaesthetic time but this may increase costs.
- Time in hospital 5-10 days
- Larger operation so potentially more risks associated.
Post Operative Care:
- No driving for 3-5 weeks
- No heavy lifting for 6 weeks.
Tram Flap
- Free flap surgery – The surgeon disconnects the tissue completely from its blood supply and reattaches the tissue to new blood vessels near your chest. Because of reattaching blood vessels, free flap surgery typically takes longer than does pedicled flap surgery. (see below images)
- Other areas of the body are the back (Latissimus Dorsi Flap) and the buttock (Inferior Gluteal Flap), amongst others. These areas have much less tissue to move and therefore may also require prosthesis to improve volume of the reconstructed area. (see below image)
Autologous reconstruction is restricted by lack of adequate donor tissue with appropriate blood supply, and adequate volume. Lack of good vessels can be due to congenital deficiency or previous surgery in the donor area. Adequate blood supply is critical to the survival of transplanted tissue in flap surgery, hence it may be preferable not to perform a pedicled flap procedure if you’re a smoker or if you have diabetes, vascular disease or a connective tissue disorder.
This form of reconstruction can be immediate (at the time of the mastectomy) or delayed (as a separate procedure some time after the mastectomy). Sometimes a better aesthetic approach is staged which means that some reconstructive surgery is done at the same time as the mastectomy and some being done as delayed reconstruction.
The donor site for the tissue used for your flap reconstruction depends on a number of factors, including:
- Body type – If you have enough extra tissue in one place to recreate the breast, the location of that tissue can influence the type of flap reconstruction you have. For example, if you are thin, you may not have enough extra tissue on your belly for a TRAM or DIEP flap.
- Breast size – If your breasts are large, you may have to use the donor site that has the most available extra tissue. In these instances a flap reconstruction could be combined with an implant.
Things to know about flap reconstruction: The physical effects of each type of autologous reconstruction are highly individual to your body, your range of motion, your physical strength, and your normal day-to-day activities.
- Remember that while you’re healing from surgery, there will be at least two and perhaps four areas of the body that are healing at the same time — your reconstructed breast(s) and the donor tissue site(s), depending on whether one or both breasts are being reconstructed at the same time. Some women may also have a sentinel node biopsy or axillary node dissection at the same time, which means an additional incision.
- With all types of reconstruction (implant and flap), there is no “one and done” option: There is nearly always a later surgery to make adjustments, sometimes called “finishing work.” Examples include nipple reconstruction, reshaping a flap, removing extra fat from a donor site, or repositioning of an implant.
- If you gain or lose weight, the size of a flap reconstruction can change along with the rest of your body. The breast(s) will get larger or smaller as your body changes.
- Flap reconstructions tolerate radiation therapy better than implants alone do. If radiation is part of your treatment plan, make sure to discuss this with your surgeon.
- Once tissue is used to build a flap, tissue from that same area cannot be used again in the future.
- In general, flap breast reconstruction surgery is more extensive than is mastectomy or implant reconstruction. Flap procedures result in larger incisions that take longer to heal, so they require a longer recovery period and may require a longer hospital stay.
Potential Complications
Breast reconstruction with flap surgery is a major procedure and carries with it the possibility of significant complications, including:
- General anaesthetic risks – Cardiac, Respiratory, Deep Vein Thrombosis
- Changes in breast sensation
- Prolonged time in surgery and under anaesthesia
- Extended recovery and healing time
- Poor wound healing
- Fluid collection (seroma)
- Infection
- Bleeding
- Tissue death (necrosis) due to insufficient blood supply
- Loss of sensation at the tissue donor site
- Abdominal wall hernia or weakness
- Keloid scar
Keep your expectations realistic about your surgery. Breast reconstruction offers many benefits, but it won’t make your breast look or feel exactly like it did before your mastectomy.
What breast reconstruction can do:
- Give you a breast contour
- Help your breasts look natural under clothing or a bathing suit
- Help you avoid the need for an external prosthesis which sits inside your bra
What breast reconstruction might do:
- Improve your self-esteem and body image
- Partially erase the physical reminders of your disease
- Require additional surgery to correct reconstructive problems
What breast reconstruction won’t do:
- Make you look exactly the same as before
- Give your reconstructed breast the same sensations as your normal breast