Management of the Axilla
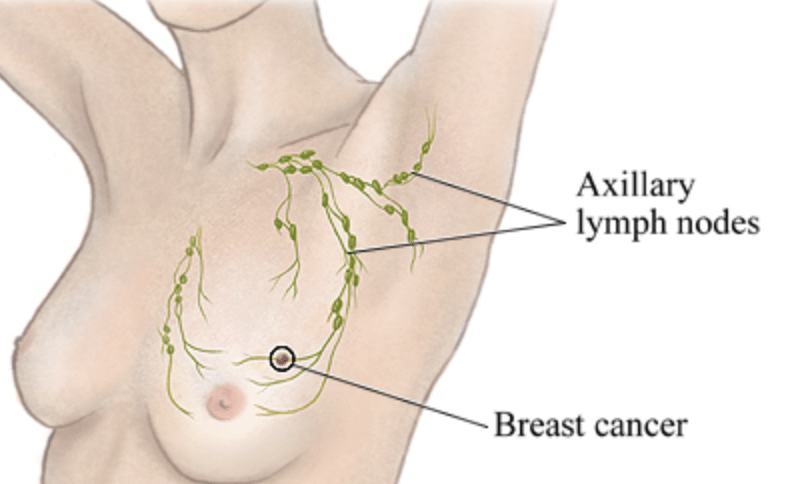
It is important to assess the main drainage system of the breast to assess whether there is any spread of invasive cancer. Assessment of tumour in the lymph nodes is important as it allows control of the cancer just outside the breast prior to spread elsewhere in the body, and the ability to Stage the cancer for further treatment advice such as chemotherapy and radiation therapy. It also assists with prognostic data.
The majority of the drainage of the breast (85%), will tend to move via the lymphatics to the lymph nodes situated under the armpit on the same side.
Traditionally this was completely cleared as in an axillary clearance, where all lymph nodes are removed from the armpit on the same side as the breast cancer. This procedure carries with it the potential complications of seroma (ongoing fluid collection), lymphoedema (swelling of the arm), shoulder stiffness, paraesthesia (pins and needles sensation or numbness of the armpit or upper arm).
Currently, the lymph nodes are initially assessed by both clinical examination and ultrasound. If a lymph node appears suspicious on ultrasound, a biopsy is performed under ultrasound guidance using a fine needle to suck out cells and check them under a microscope for cancer cells.
During an Ultrasound guided fine needle aspirate you will be lying on your back, tilted to one side, on the couch in ultrasound room, with the upper body undressed. The arm on the side of interest will be raised above the head. Antiseptic solution is used to clean the skin and then gel will be inserted over the skin and the ultrasound probe placed on top to find the lymph node of interest. Local anaesthetic may or may not be used. The needle is inserted into the lesion and the radiologist will make several small (less than 1 cm) forward and backward gently movements with the needle to collect cells.
If this is negative for disease, then a sentinel node biopsy is performed looking for microscopic deposits.
Sentinel Node Biopsy
The sentinel lymph node(s) is the first draining node within a basin of approximately 20 lymph nodes.
Sentinel Node Biopsy is a technique used to assess for small amount of cancer in the lymph nodes under the armpit (axilla) without having to remove all the lymph nodes (axillary dissection), and hence decreasing the potential complications of Axillary Clearance, which may be an unnecessary procedure.
If the sentinel node does not contain cancer, as in 80% of all early breast cancers, then there is no requirement to remove the rest of the lymph node basin (axillary clearance).
If the sentinel node contains cancer, it will depend on the amount of disease present as to whether it is oncologically necessary to clear the rest of that lymph node basin. In other words, proceed with an Axillary Clearance.
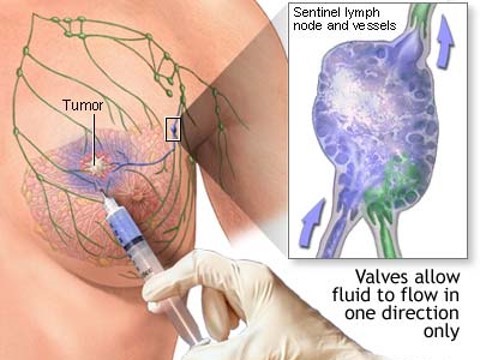
The Sentinel Node is located by injecting one or two dyes around the periareolar margin or around the tumour site, just prior to surgery.
Details
Potential Complications:
- Bleeding
- Wound Infection
- Seroma (fluid collection) – usually minimal
Post Operative Care:
- Keep wound dry
- No driving /heavy lifting for 2 weeks
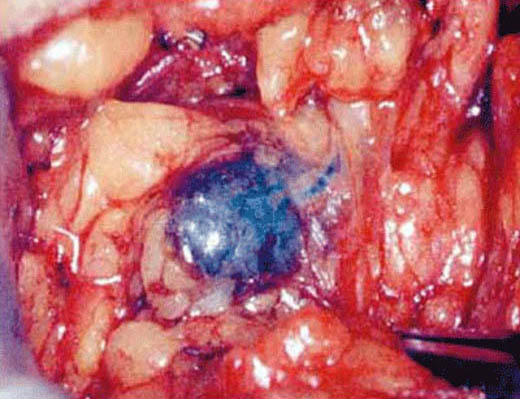
The dyes used are radioactive and patent blue dye, and the sentinel node is detected using a gamma probe to find a focus of radioactivity, as well as visually looking for a blue lymph node. There are now emerging techniques using a magnetic tracer to find iron particles, and visually looking for carbon particles.
The sentinel nodes are checked for metastatic disease. Depending on the numbers involved and the size of the cancer deposit (< 3mm) the decision to complete an axillary dissection (removal of ALL the lymph nodes, within the axilla) is made.
The accuracy of this technique is 97%. The false negative rate 7%-12%. These figures can be obtained only by a surgeon well trained in this area.
The sentinel nodes are checked for metastatic disease. Depending on the numbers involved and the size of the cancer deposit (< 3mm) the decision to complete an axillary dissection (removal of ALL the lymph nodes, within the axilla) is made.
The accuracy of this technique is 97%. The false negative rate 7%-12%. These figures can be obtained only by a surgeon well trained in this area.
Procedure
Under general anaesthesia, inject the dye periareolar (around the nipple-areolar complex) during the actual breast surgery or prior as a single stand alone procedure.
Minimally invasive with either a small incision (1.5-2.5cm) under the armpit, or accessible through the breast incision for removal of the breast cancer.
Precise location can be achieved with little trauma to the surrounding tissue using the localisation techniques of a gamma probe and visualising the blue dye.
No drains required.
If performed solitary, only requires only a day stay. If performed in conjunction with breast surgery, follow post operative advice of the breast surgery.