Precancerous breast conditions typically do not present with any breast symptoms. They are typically picked up incidentally on breast imaging for an unrelated breast symptom or on general breast cancer screening. A biopsy confirms the diagnosis.
The different precancerous breast lesions are atypical ductal hyperplasia (ADH), atypical lobular hyperplasia, atypical columnar cell hyperplasia or flat epithelial atypia (FEA), ductal carcinoma in situ (DCIS), lobular carcinoma in situ, papillary lesions, and proliferative radial scar.
Atypical hyperplasia
It is not clear what causes atypical hyperplasia.
Atypical hyperplasia forms when breast cells become abnormal in number, size, shape, growth pattern and appearance. The appearance of the abnormal cells determines the type of atypical hyperplasia:
- Atypical ductal hyperplasia describes abnormal cells within the breast ducts.
- Atypical lobular hyperplasia describes abnormal cells within the breast lobules.
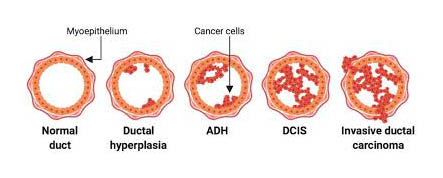
Atypical hyperplasia is thought to be part of the complex transition of cells that may accumulate and evolve into breast cancer. The progression to breast cancer typically involves:
- The process begins when normal cell development and growth become disrupted, causing an overproduction of normal-looking cells (hyperplasia).
- Atypical hyperplasia. The excess cells stack upon one another and begin to take on an abnormal appearance.
- Noninvasive (in situ) cancer – DCIS. The abnormal cells continue to progress in appearance and multiply, evolving into in situ cancer, in which cancer cells remain confined to milk ducts.
- Invasive cancer. The abnormal cells accumulate within the duct and continue to multiply and transition to become cancer cells. Invasive cancer tends to invade surrounding tissue, blood vessels or lymph channels.
Risk Factors
Factors that may increase your risk of DCIS include:
- Increasing age
- Personal history of benign breast disease, such as atypical hyperplasia
- Family history of breast cancer
- Never having been pregnant
- Having your first baby after age 30
- Having your first period before age 12
- Beginning menopause after age 55
- Genetic mutations that increase the risk of breast cancer, such as those in the breast cancer genes BRCA1 and BRCA2
Once diagnosed with atypical hyperplasia, you have a risk factor that increases your risk of developing breast cancer in the future. The risk of breast cancer in those with atypical hyperplasia is about four times higher than in those who do not have hyperplasia.
The breast cancer risk with women with atypical hyperplasia increases over time:
- At 5 years after diagnosis, about 7% of women with atypical hyperplasia may develop breast cancer. Put another way, for every 100 women diagnosed with atypical hyperplasia, 7 can be expected to develop breast cancer five years after diagnosis. And 93 will not be diagnosed with breast cancer.
- At 10 years after diagnosis, about 13% of women with atypical hyperplasia may develop breast cancer. That means for every 100 women diagnosed with atypical hyperplasia, 13 can be expetected to develop breast cancer 10 years after diagnosis. And 87 will not develop breast cancer.
- At 25 years after diagnosis, about 30% of women with atypical hyperplasia may develop breast cancer. Put another way, for every 100 women diagnosed with atypical hyperplasia, 30 can be expected to develop breast cancer 25 years after diagnosis. And 70 will not develop breast cancer.
Ductal Carcinoma In Situ – DCIS
Ductal carcinoma in situ (DCIS) is the presence of abnormal cells inside a milk duct in the breast.
It is considered the earliest form of breast cancer. DCIS is non-invasive, meaning it hasn’t spread out of the milk duct and has a low risk of becoming invasive, and therefore if removed, has an extremely good outcome
DCIS is usually found during a mammogram by detecting small clusters of calcifications that have irregular shapes and sizes.
DCIS presents in 3 grades – low, intermediate, and high. Both intermediate and high grade is known to progress to an invasive cancer and therefore is highly advisable to be removed to prevent a full cancer from occurring. Treatment may include breast-conserving surgery (wide local excision) combined with radiation, or surgery to remove all the breast tissue (mastectomy) with or without reconstruction.
It is not clear exactly what causes DCIS. DCIS forms when genetic mutations occur in the DNA of breast duct cells. The genetic mutations cause the cells to appear abnormal, but the cells do not have the ability to break out of the breast duct.
Factors that may trigger the abnormal cell growth that leads to DCIS include your lifestyle, your environment and genes passed to you from your parents.
Papillary lesion – Papilloma
Papillomas: These small outgrowths from the lining of the mammary milk ducts, commonly near the nipple. The often present as nipple discharge, either clear or bloody. Sometimes they can present as a breast lump, usually close to the nipple.
Most intraductal papillomas are non-cancerous, however 17-20% have been shown to be cancerous upon complete removal of the growth. In addition, about 20% of intraductal papillomas contain abnormal cells. Because there is even a small risk of cancer, papillomas should be surgically removed and biopsied.
Management includes a clinical examination, nipple discharge biopsy for cytology, ultrasound and/or mammography. Biopsy of the tissue should be performed under ultrasound guidance to confirm the diagnosis
Surgery is the recommended treatment to remove the papilloma even if the biopsy suggests it is benign, so that the whole growth can be evaluated for any indications of cancer, and to remove it prior to it turning into a cancer.
Radial Scar
Radial scars and complex sclerosing lesions are benign (not cancerous) conditions. They are the same thing but are identified by size, with radial scars usually being smaller than 1cm and complex sclerosing lesions being more than 1cm.
A radial scar is a growth that looks like a cancer on a mammogram or ultrasound. It does not present with any breast symptoms. When the tissue is viewed under a microscope it looks like a scar. It has a central core containing benign ducts. Growing out of this core are ducts and lobules that show evidence of unusual changes such as cysts and epithelial hyperplasia (overgrowth of their inner lining).
The reported prevalence of radial scars is 0.1-2.0 per 1,000 screening mammograms. A radial scar is most often seen in women between 41-60 years
Sloane and Meyers reported a 30% incidence of carcinoma on follow up, when the radial scar measures 6 mm or larger
Treatment of radial scars/complex sclerosing lesions should therefore be preventative excision.
Columnar Cell Change
With the increasing use of mammography screening scans in the last 30 years, columnar cell lesions (CCLs) have been diagnosed more frequently, often associated with microcalcifications and abnormal calcifications which require breast biopsies.
Progression of these lesions to invasive cancer has been reported as increasingly low (2–7%). This arises controversy to the management of those lesions. Currently it is not advised to excise all, but to keep closer breast surveillance in the area they were found.